
As women approach their mid-40s and early 50s, they often begin to experience the transitional phase known as perimenopause. This stage happens before the onset of menopause and is characterized by a variety of physiological changes, one of the most significant being bone density loss. Understanding the connection between perimenopause and bone density loss is crucial for preventing long-term complications and maintaining your overall health. In this blog, we will explore the impact of perimenopause on bone health, the role of BMD (bone mineral density), and practical strategies to manage and mitigate bone loss during this critical period.
What Happens During Perimenopause?
Menopausal transition, commonly known as perimenopause, can start several years before menopause. It starts with fluctuations in hormone levels, particularly estrogen, which play a vital role in maintaining bone health. Estrogen helps regulate the bone remodelling process, where old bone is replaced by new bone tissue. As estrogen levels decline during perimenopause, this balance is disrupted, leading to an increased risk of bone density loss.
Symptoms of Perimenopause
Common symptoms of perimenopause include:
- Irregular menstrual cycles
- Hot flashes
- Night sweats
- Mood swings
- Sleep disturbances.
However, one of the less obvious but equally critical changes occurring during this time is the reduction in bone mineral density. This decline can lead to weaker bones, making women more susceptible to fractures and osteoporosis.
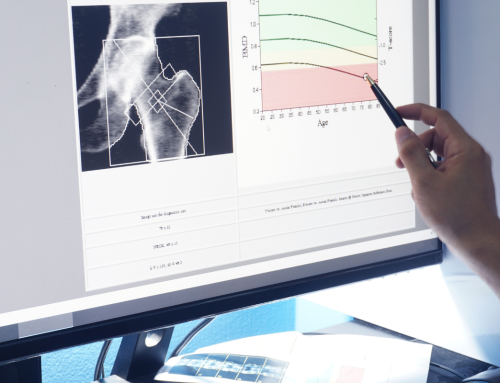
The Importance of BMD Bone Mineral Density
Bone Mineral Density (BMD) measures the amount of minerals, primarily calcium, contained in a specific volume of bone. It is a critical indicator of bone strength and health. During perimenopause, monitoring BMD becomes essential to assess the risk of bone-related conditions and take preventive measures.
Why BMD Matters
Understanding the significance of BMD is essential for maintaining bone health and preventing serious conditions. Here is why you should talk to your doctor about BMD testing if you’ve entered perimenopause:
- Early Detection of Osteoporosis: BMD tests will flag osteoporosis in its early stages, allowing for timely intervention and treatment to prevent fractures.
- Fracture Risk Assessment: Low BMD is a significant risk factor for fractures. Understanding your BMD can help you take steps to protect your bones and reduce the risk of injury.
- Monitoring Bone Health: Regular BMD assessments can track changes in bone density over time, providing valuable information on the effectiveness of lifestyle changes and treatments.
Factors Contributing to Bone Density Loss During Perimenopause
Several factors contribute to bone density loss during perimenopause, including hormonal changes, lifestyle choices, and genetic predispositions. Let’s dive into the details.
Hormonal Changes
The decline in estrogen levels during perimenopause is the primary driver of bone density loss. Estrogen helps balance bone resorption (breakdown) and bone formation. With reduced estrogen, bone resorption outpaces bone formation, leading to a net loss of bone density.
Lifestyle Factors
Certain lifestyle choices can exacerbate bone density loss during perimenopause:
- Diet: A diet low in calcium and vitamin D can contribute to bone density loss. Calcium is crucial for bone health, and vitamin D helps the body absorb calcium effectively.
- Physical Activity: Lack of weight-bearing and resistance exercises can weaken bones. Regular physical activity is essential for maintaining and improving BMD.
- Smoking and Alcohol: Smoking and excessive alcohol consumption can negatively affect bone health, accelerating bone density loss.
Genetic Predispositions
Genetics also plays a role in determining bone density. If you have a family history of osteoporosis or fractures, you may be at a higher risk and should consider regular BMD testing.
Strategies to Mitigate Bone Density Loss During Perimenopause
While the hormonal changes of perimenopause are inevitable, there are several strategies women can adopt to mitigate bone density loss and maintain overall bone health.
Nutrition and Supplements
A balanced diet rich in calcium and vitamin D is crucial for bone health. Aim to include the following in your diet:
- Calcium-rich foods: Dairy products, leafy green vegetables, fortified plant-based milk, and tofu.
- Vitamin D Sources: Fatty fish, fortified foods, and supplements if necessary. Vitamin D helps the body absorb calcium and is essential for bone health.
Regular Exercise
Regular physical activity, particularly weight-bearing and resistance exercises, can help improve BMD. However, you don’t need heavy-hitting workouts that leave you breathless. Walking, jogging, weightlifting, and yoga are excellent for maintaining bone health.
Lifestyle Modifications
Living a healthy lifestyle benefits more than just your bones, but here’s how making a few minor adjustments can help mitigate bone loss.
- Quit Smoking: Smoking cessation is vital for bone health as smoking reduces blood flow to the bones, which can decrease bone density.
- Limit Alcohol: Reducing alcohol consumption can help maintain the balance of calcium and vitamin D in the body, supporting bone health.
Medical Interventions
Sometimes, medical interventions may be necessary to address significant bone density loss. Hormone Replacement Therapy (HRT) and other medications can help maintain bone density during perimenopause. Consult with your doctor to determine the best approach for your individual needs.
Understanding the link between perimenopause and bone density loss is crucial for maintaining overall health and preventing long-term complications such as osteoporosis. Women can effectively manage bone health during this transitional period by monitoring BMD bone mineral density and adopting lifestyle changes.
For those seeking additional support, innovative technologies like the Marodyne LiV device offer a safe, patent-pending, scientifically established solution to naturally enhance muscle strength, function, and circulation, thereby supporting and improving BMD. Investing in such a device can promote better bone health and a higher quality of life during perimenopause and beyond. Embrace the opportunity to take control of your bone health with Marodyne LiV and experience the benefits of improved muscle strength and circulation naturally and safely. Contact us to chat more about the device that can enhance your health.
What surprised you about the link between perimenopause and bone density loss? What’s something you can do to help mitigate bone loss as you age? Share your thoughts with our readers in the comments below.



 Black Friday → Christmas Sale! Save $300 + Free Shipping
Black Friday → Christmas Sale! Save $300 + Free Shipping 